A Thorough Examination
Some of you may recall Vanisha’s article from April this year - ‘Put Your Best Foot Forward’ - in which she explained the anatomy of our feet and outlined some of the common foot issues we see at the Practice. One of the conditions she mentioned was plantar fasciitis; a painful condition that affects the base of the foot, which can last for years if not managed correctly.
It so happens that I have had a number of patients presenting with this condition recently. So, I wanted to expand on this particular aspect of Vanisha’s article and go into more depth about the causes, symptoms and chiropractic treatments that we can offer here at Creative Chiro. I will also offer an in-depth insight into the process of getting to the root cause of complicated issues such as this.
When it comes to foot problems, life goes on even if you are limping along in pain! In the presence of discomfort that causes you to alter your gait (the way you move) and limp, you will still be able to move around and carry on with your life to some degree. So, people will tend to just soldier on hoping it will get better over time.
However, that limp is happening for a reason which, in many cases, can be resolved if the root cause is found and a correction made. Badly fitting shoes, verrucas, bunions, gout, splinters, flat feet, trauma, athlete’s foot and numbness can all cause an adaptation in your gait which, if unresolved, can affect almost every other part of your body.
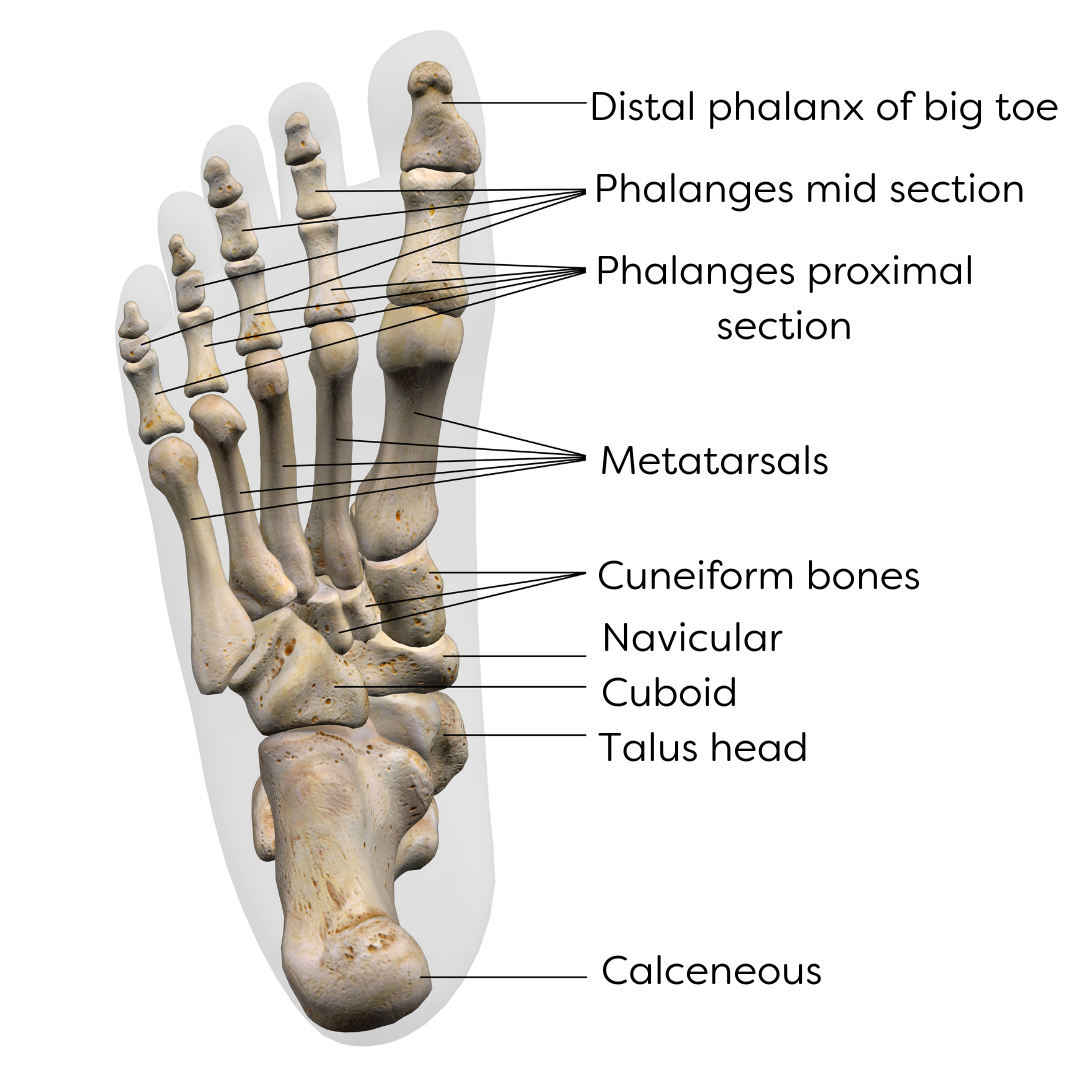
Before we go on, here is a little anatomy lesson…
Plantar and dorsum are the two words used to describe the upper and lower surfaces of the foot. The dorsum relates to the top part of the foot, sometimes called the bridge. Conversely, the plantar surface is the underneath of the foot, commonly known as the arch.
So, first things first – what is plantar fasciitis?
Well, the clue is in the name. So, let us start with the word, ‘plantar.’ This area - shown above - has muscles which maintain the integrity of the arch of the foot, aiding stability and balance. This allows the arch to flatten when walking, to distribute the weight-bearing load created upon impact with the floor.
Next is ‘fasciitis.’ This is really two words, fascia, and itis.
Fascia is a thin, cobweb-like material that forms a casing of connective tissue, which surrounds and supports every organ, blood vessel, bone, nerve fibre and muscle in the body. It plays a crucial role in maintaining your bodily structure, allowing for smooth movement, contributing to overall physical and emotional well being. Fascia is also a sensory-rich tissue, comprising of nerves that make it almost as sensitive as skin.
Itis means ‘inflammation.’ If we put it all together, plantar fasciitis means ‘inflammation of the connective tissue in the sole of the foot’ …and boy, can it be painful!
Symptoms of plantar fasciitis
The main symptom of plantar fasciitis is pain in the underside of the foot, around the heel and into the arch. There can be other reasons for this discomfort, but it is more likely to be plantar fasciitis if the following apply:
1. The pain is much worse when you first start walking, after getting out of bed or sitting for a while.
2. It gradually feels better when you start moving around, but then gets worse if you stand, walk or run for a prolonged period of time.
3. It is painful when stretching the bottom of your foot, such as when raising your toes off the floor or walking up stairs.
What can you do to alleviate these symptoms?
There are some things you can do to help yourself, such as stretching your feet on the bottom run of a stair, massaging the bottom of the foot by standing and rolling the arch on a frozen golf ball or through more drastic measures such as painkilling or anti-inflammatory injections. However, when patients present to the practice having tried a plethora of self-help ideas and the symptoms keep returning, it is always the case that the symptoms have been targeted but the root cause of the issue has not been identified.
How can chiropractic treatment help with plantar fasciitis?
Another quick anatomy lesson…
This always seems to be a good pub quiz question: ‘How many bones are there in the foot?’
There are 26 bones altogether. 7 bones make up the ankle and these are called the calcaneus, talus, cuboid, navicular and three cuneiforms.
The ankle joint is formed by the talus articulating with the end of your shin. All of these bones and joints have to work independently of one another, but also operate together to create the perfect foundation for you to walk correctly. If any one of these becomes fixed or painful, the rest have to adapt in some way. This can cause unequal loading through the muscles of the foot, leading to plantar fasciitis. In addition, this can affect the achilles tendon and calf and so progress further up the leg to the hip and back.
Chiropractors are typically known for treating issues that arise in the spine. However, if you are suffering from a problem that causes you to limp, this can be the very reason why spinal discomfort develops in the first place. Therefore, if the unwise just focus on the area of pain without looking elsewhere, the real issue that needs to be dealt with can be missed.
The feet are the foundations of your body and - like building a house - if you start with a poor foundation, you will tend to struggle with the rest of the build. Hence, every new patient we see at Creative Chiro starts by having their gait assessed even though they may be coming in with a history of neck, shoulder or back problems which, seemingly, have nothing to do with the feet.
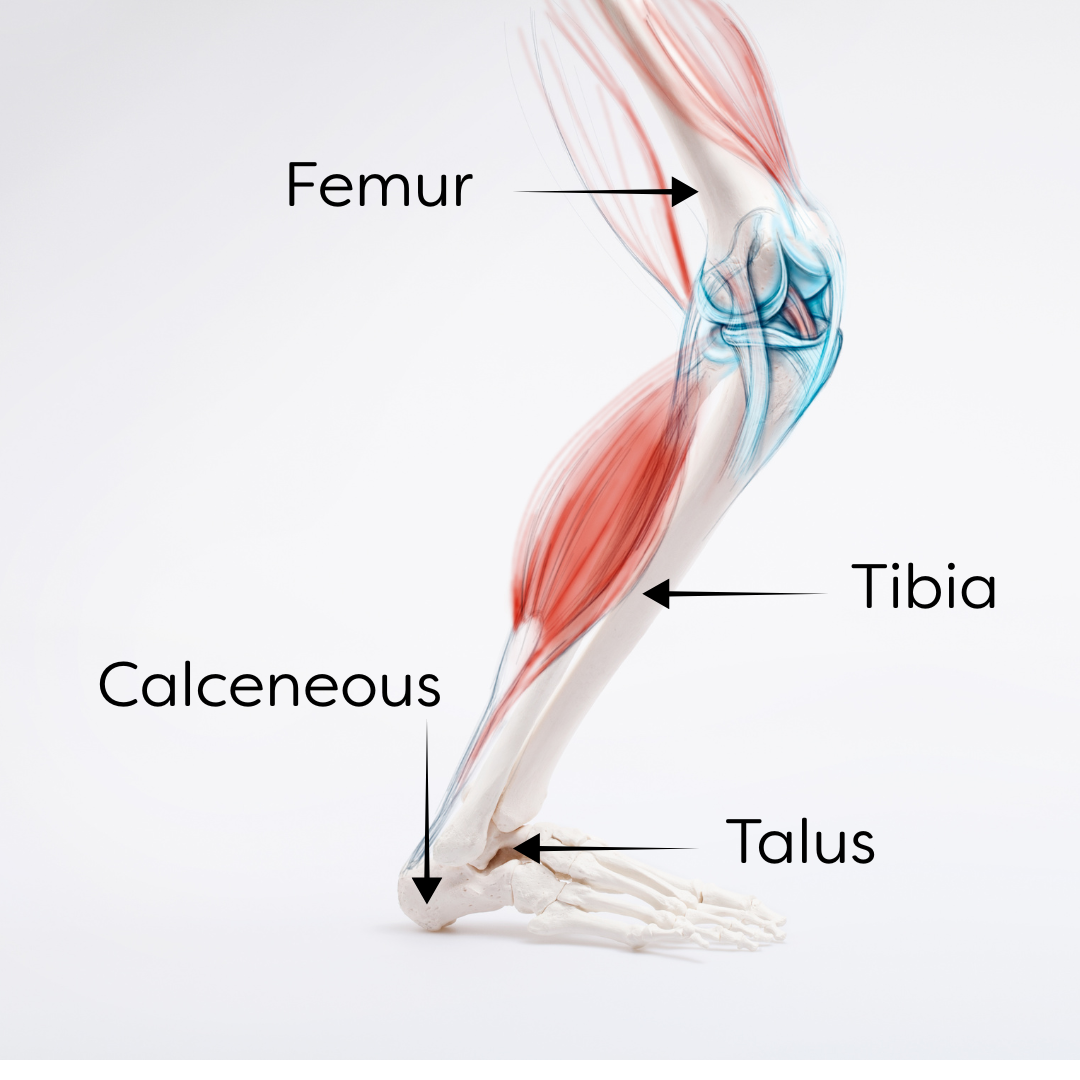
In addition to this, chiropractors look at the body as a series of links or, to be technical, ‘kinetic chains.’ A kinetic chain is an interconnected system which involves the muscles, bones, ligaments and tendons that work together to produce movement. In this instance, we are referring to the kinetic chain of the lower limb and like any chain, its strength is dictated by the weakest link which, if it fails, results in the whole chain failing. Therefore, if the foot is the weakest link in the system, the whole leg will fail to function correctly, causing all manner of problems in the rest of the body.
The main bones involved in the kinetic chain of the lower leg when walking are the femur, tibia, talus and calcaneous bones, as shown here.
This kinetic chain concept is quite an amazing process, a little like a domino effect, which I will attempt to describe below:
The kinetic chain starts the moment your heel strikes the floor.
This strike force causes the heel bone (calcaneus) to rotate outwards (eversion).
This makes the bone connecting your ankle to your leg (talus) to move slightly forward.
This results in the shin bone (tibia) rotating outwards, causing the knee to deviate slightly inwards.
This causes the thigh bone (femur) to turn outwards, resulting in the major stabilising muscle in the buttock (gluteus medius) switching on, so that you do not fall over when you walk!
This process should occur with every stride you take and it is why we first look at a patient’s gait when we assess for any musculoskeletal problems.
Assessing the presenting patient
When a patient arrives with soreness underneath the foot, they have often tried a myriad of other treatments to try and solve their debilitating pain. They may have done their own research online which is not always reliable, as we all know. However, it is important that the patient is given time to talk through their thoughts and ask questions about their problem. We then start the process of examination, which begins by simply watching and listening to the way they move around the consulting room. This can produce a wealth of information and we have not even laid hands on the patient yet!
For instance, we can see if a patient:
Over-strides
Walks in a cross-over style
Over pronates (has a collapsed arch, known as pes planus)
Has hallux valgus (a bunion)
Has a valgus knee (knock knees)
Has a varus knee (bow legged)
Has a high arch (known as pes cavus)
Lifts the heel prematurely off the floor (indicating a tight calf especially if the knee is bent)
Has a collapsing gait (known as a Trendelenburg sign)
And the list goes on and on! But hopefully you get the gist! All we have done is observe and already we have plenty to get our teeth into.
We will now have a good idea of what is going on. Next, we need to do a physical examination to assess movement patterns and potential restrictions in the way the joints, muscles ligaments and tendons of the knee, ankle and foot interact with each other.
After thoroughly assessing all of these factors, we can then make a sound clinical judgement and produce a working diagnosis of exactly what is going on. More importantly, we also now know what we are going to do as far as treatment is concerned. This will involve advising the patient about the dos and don’ts of their aftercare. The best way of explaining this is through a working example…
A case study
Patient history: Trudy, an active person in her fifties, presented recently with a four-week history of intense pain in the sole of her right foot, which had been gradually getting worse. She felt she had all the correct footwear. She had not suffered any recent traumas. There was no one incident she could recall that ‘set it off’, but almost all of her activities of daily living were now affected.
She had no pain to her back or thigh but the pain in her foot had migrated into her calf. She had no numbness or pins and needles into the leg or foot and she was still able to do all of her stretch exercises from Pilates without any problems.
She had recently been diagnosed by another health professional with ‘achilles tendinopathy’ (an overuse injury to the tendon that connects the lower leg to the heel). She had been given exercises to do and told it would ‘go away with time’ and that not much more could be done, other than purchase some shoe inserts from the local chemist.
Examination: Trudy had a clear limp from the right foot and had a shortened stride. The very heavy heel strike of the left foot indicted this point. No flat feet were evident. Getting Trudy to do alternate one-leg squats, I observed a weakness to her right gluteus medius muscle in her buttock. She was unable to walk on her heels and toes without pain.
With Trudy laying face up on the treatment table I examined her lower limb neurology to check for nerve problems. Her hips, basic leg strength and movement patterns were all fine. However, there was an indication of an issue with the outside of her right knee. This was due to restricted movement of the fibula bone in her lower leg, which caused pain to the outer part of her calf.
I then examined her ankle and foot. There was clear discomfort within the muscles in the sole of her right foot, with a marked degree of spasm. The area just above the ankle and along the achilles tendon was swollen and sore to touch. There was no evidence of any bunions and the toes moved easily and pain-free. However, movement of the right ankle had several issues with the heel bone (calcaneus) totally locked and unable to rotate either way. The bone on the outside of the ankle (cuboid) was equally stuck, with tenderness through the connective tissues up into the other end of the fibula. The bone in the inside of the ankle that forms the top of the foot arch (navicular) was the main issue and any amount of pressure applied there made Trudy wince.
From this examination, it was a clear, text-book case of right plantar fasciitis, but with some added compensatory issues into the achilles tendon, calf and fibula.
Treatment: For those of you who are not familiar with the corrective methods chiropractors use to manage presentations such as Trudy’s, in essence, we use controlled manipulative procedures to get the areas that are stuck to move again. In this case, Trudy’s right calcaneus, navicular, cuboid and both ends of the fibula were manipulated using one of the many techniques at our disposal called ‘toggle’. This uses a professional piece of equipment and is not painful for the patient.
Re-examination: I work within a branch of medicine where I am fortunate to witness some amazing results and Trudy’s case was one of them. After treatment, she could walk around with what she described as a 75% reduction in pain. there was no longer an apparent limp and there was a better stride pattern, with an even heel strike. Walking on her toes was fine, but still a little uncomfortable on her heels. There was no collapsing of the gluteus medius upon doing the one-leg squat and the pain had virtually gone from her right achilles.
Aftercare: I advised Trudy to use an ice pack to the achilles if it became sore and to stretch the achilles, but only in a relatively pain-free manner. This was to be done on the lower step of the stairs, holding herself steady with the handrail with the front half of the foot on the step. With knees locked, Trudy was instructed to go up on her toes and then stretch her foot down as far as possible, fifteen times. Then to repeat this, but while maintaining around a 20-degree bend in the knees. Again, up on the toes and stretch down fifteen times with these bent knees.
This is designed to stretch the two muscles in the calf (gastrocnemius and soleus) whose tendons come together to form the achilles tendon. Trudy was pain-free after three treatments. Ongoing advice was given about her shoes and she was advised not to tie her laces too tightly!
In conclusion…
Plantar fasciitis is a very common condition that - in many cases - can be helped. In her own words, Trudy said that: “I got my life back from what you have done!” - For me, this says it all and it put a big smile of my face as I drove home at the end of that day.
So, is every chiropractic patient fixable? Absolutely not! However, in the majority of cases, patients do benefit from our care. I am not someone who shouts from the rooftops about what we do. We are very grateful to have an army of patients who do that for us.